All news by therapy
2024
24
APR
Why breath-by-breath built-in software data should be used to monitor CPAP/NIV in children?
Last February, an interesting Letter to the Editor regarding the importance of using "Breath to Breath" detailed data obtained from ventilator software for the long-term follow-up and monitoring of children on non-invasive ventilation (CPAP/NIV), was published on Pediatric Pulmonology.
For children undergoing continuous positive airway pressure (CPAP) or non-invasive ventilation (NIV) therapy, proper follow-up is important to assess therapy adherence, leaks, ventilation adequacy, and any residual respiratory events.
The gold standard for monitoring is polysomnography/poligraphy (PSG/PG) during ventilation, but access to PSG/PG is limited and not available in all pediatric centers. Therefore, in recent years, there has been increasing use of alternatives such as nocturnal oximetry monitoring and transcutaneous CO2 monitoring along with analysis of data from CPAP/NIV device software.
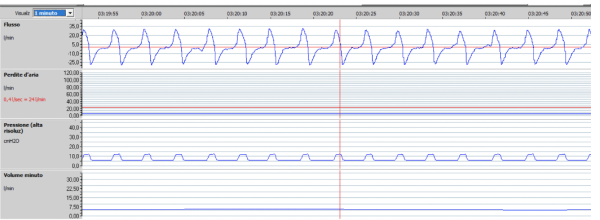
While the analysis of these software data to evaluate adherence, volume trends, respiratory rate, and leaks is becoming more common, the analysis of breath-to-breath traces is still rarely used. However, it is crucial for detecting real or false residual respiratory events and adjusting device settings to maximize treatment effectiveness.
In the case of patients on NIV, patient-ventilator asynchronies (PVA) are a well-known phenomenon and can be identified through breath-to-breath analysis. PVAs include trigger asynchronies, cycling asynchronies, unintentional leaks, respiratory rate asynchronies.
Correction of unintentional leaks and adjustment of device settings are crucial steps in managing PVAs.
In the case of patients on CPAP, breath-to-breath analysis of traces, ideally with simultaneous SpO2 monitoring, can detect "real" residual respiratory events or rule out false events caused by inappropriate airflow detection. Therefore, the detection of significant residual respiratory events should lead to an increase in CPAP level. If possible, integrating analysis of thoraco-abdominal belts connected to the ventilator can provide additional useful information to characterize residual respiratory events.
The article provides interesting practical examples.
The authors conclude that adapting ventilator settings and reviewing integrated software data can generally manage most residual respiratory events and PVAs in children on CPAP or NIV.
However, further research is needed to fully understand the effectiveness of this strategy and compare it with the traditional approach using PSG/poligraphy.
BIBLIOGRAPHY
Sonia Khirani, Marine Dosso, Lorène Gerin, Mihail Basa, Charlotte Collignon, Meryl Vedrenne-Cloquet, Lucie Griffon, Brigitte Fauroux. Why breath-by-breath built-in software data should be used to monitor CPAP/NIV in children?Pediatr Pulmonol. 2024 Feb;59(2):506-509. doi: 10.1002/ppul.26740. Epub 2023 Nov 3.
Article by Barbara Madini






